Pancreatic carcinoma
A disease of later life, pancreatic carcinoma is the third most common cancer of the gastrointestinal tract and the sixth most common cause of cancer deaths.
Pancreatic cancer is the fifth most common cause of cancer death in the UK, with an annual incidence of nearly 9,600 (1)
- on average, 23 people die each day from the disease
- UK has one of the worst survival rates in Europe, with average life expectancy on diagnosis just 4 to 6 months and a relative survival to 1 year of approximately 20%
- only 3% of people survive for 5 years or longer. This figure has not improved much in over 40 years, and it is not yet clear how the more recent trend of increased surgery and adjuvant chemotherapy will affect survival
Risk factors for development of pancreatic cancer (2)
- modifiable risk factors for the development of pancreatic cancer include, but are not limited to:
- cigarette smoking
- ∼1.7-fold increased risk compared with never smokers
- increased BMI
- ∼1.6-fold increased risk in individuals with obesity compared with those with normal weight
- diabetes mellitus
- new-onset diabetes
- <0.3–0.8% of patients with new-onset diabetes develop pancreatic ductal adenocarcinoma within 3 years of diabetes diagnosis
- long-standing diabetes
- 1.5–2-fold increased risk of pancreatic cancer for individuals with diabetes of >3 years in duration
- new-onset diabetes
- chronic pancreatitis
- twofold to threefold increased risk in individuals with long-standing chronic pancreatitis
- alcohol use
- 1.6-fold increased risk in those consuming >6 drinks per day compared with those consuming >1 drink per day
- cigarette smoking
- among the non-modifiable risk factors are:
- age
- pancreatic cancer is a disease in which risk increases with age and rarely occurs before the age of 40 years
- gender
- incidence rates for pancreatic cancer tend to be higher in men than in women, particularly in those below the age of 75 years
- family history
- twofold increased risk in individuals with a single family member with pancreatic cancer compared with the general population; sevenfold increased risk in individuals with multiple family members with pancreatic cancer compared with the general population
- hereditary pancreatitis
- genetic mutations in, for example, BRCA1, BRCA2, PALB2, ATM, CDKN2A (p16), mismatch repair genes (MLH1,MSH2, MSH6, PMS2), STK11, and PRSS1, SPINK1, and CFTR
- age
Because of late diagnosis, only approximately 8% of people with pancreatic cancer are eligible for potentially curative surgery
- however, people have up to a 30% chance of surviving 5 years if their tumour can be surgically removed and they have adjuvant chemotherapy
- symptoms of pancreatic cancer are non-specific
One survey found that 40% of people diagnosed with pancreatic cancer in England had visited their GP 3 or more times before the diagnosis was made
- fifty per cent of people are diagnosed as an emergency in A&E
70% of tumours occur in the head of the pancreas in proportion to the amount of tissue in different parts of the pancreas.
Progress is insidious. There is early regional lymph node involvement and spread to the liver. The tumour may metastasize to bone and lung.
Less common endocrine tumours of the pancreas such as glucagonomas and insulinomas may occur.
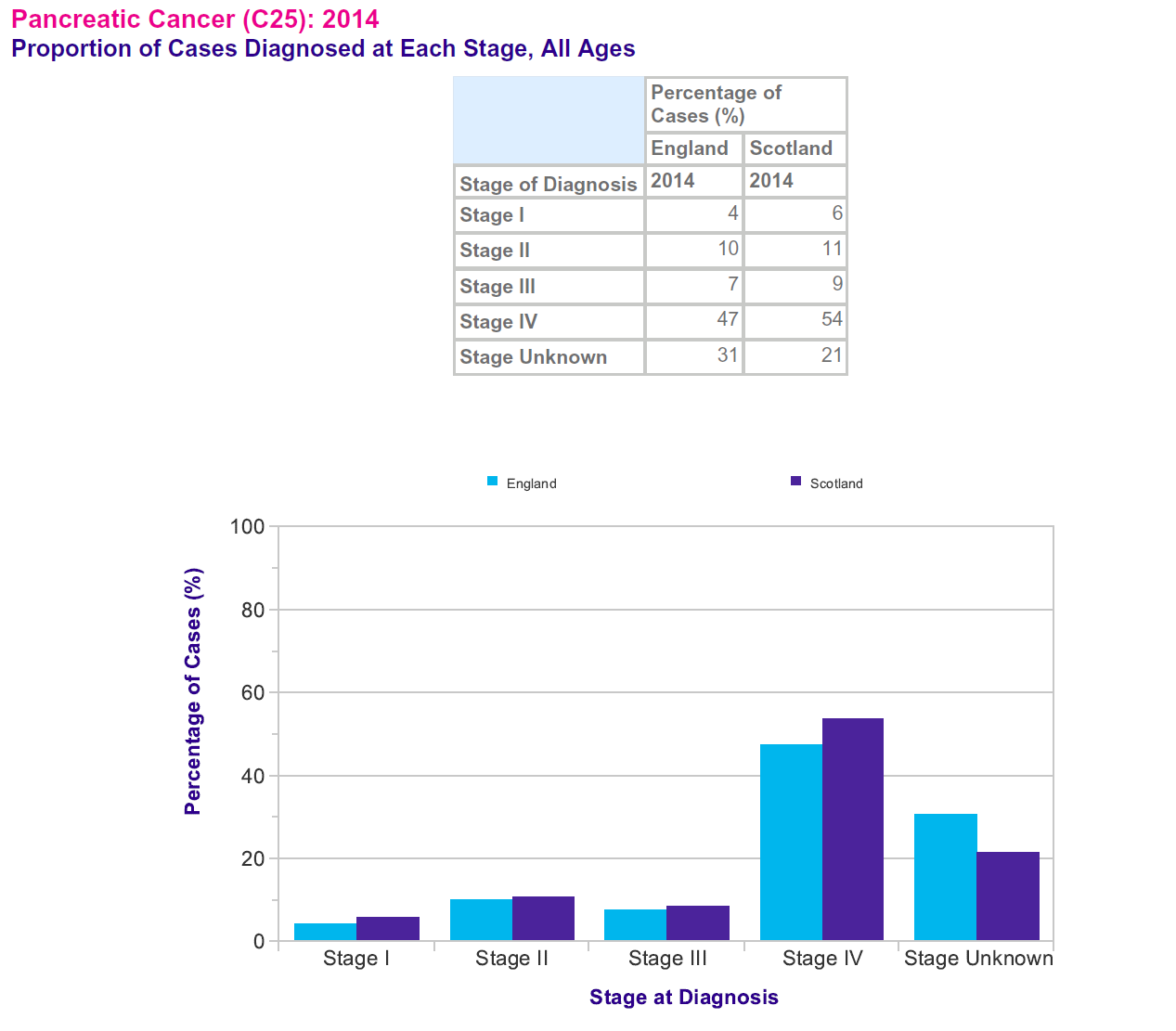
Pancreatic cancer patients with a known stage are most commonly diagnosed at stage IV (68-69%). More patients with a known stage are diagnosed at a late stage (79% are diagnosed at stage III or IV), than an early stage (21% are diagnosed at stage I or II (3)
Reference:
- NICE. Pancreatic cancer in adults: diagnosis and management. NICE guideline NG85. Published February 2018
- Klein AP. Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol. 2021 Jul;18(7):493-502.
- Cancer Research UK, Pancreatic Cancer Statistics
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.