Eosinophilia (blood)
Eosinophils account for approximately 1% to 4% of a person's leukocytes, and eosinophilia is a raised eosinophil count (1,2,3,4)
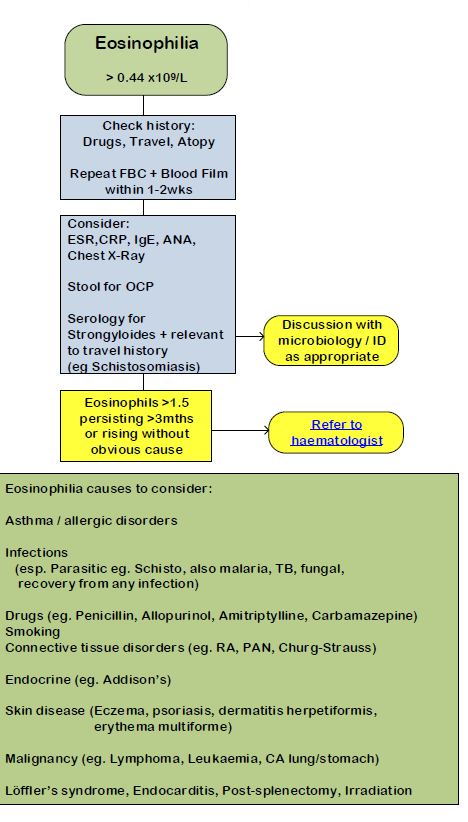
This occurs where the eosinophil count is greater than 0.44 x 109/l (3)
- however has been noted that the normal range for a peripheral blood eosinophil count in healthy individuals is generally defined internationally as 0.05-0.5×109/L (4)
- eosinophilia is a raised number of eosinophils in peripheral blood (>0.5×109/L)
- hypereosinophilia is >=1.5×109/L on two tests separated by at least one month
- eosinophil count can vary with extremes of age
- eosinophil levels are higher in neonates than adults and gradually reduce in older people.
It may be a feature of the following conditions:
- asthma and allergic disorders - asthma, hypersensitivity, drugs, angioneurotic oedema *
- parasitic infections - especially schistosomiasis, echinococciasis
- polyarteritis nodosa
- Churg-Strauss syndrome
- Addison's disease
- skin disease - pemphigus, urticaria, eczema, dermatitis herpetiformis, erythema multiforme
- malignancy:
- Hodgkin's disease
- carcinoma
- haematological malignancies:
- chronic myeloid leukaemia
- other myeloproliferative syndromes
- eosinophilic leukaemia
- Loeffler's syndrome
- Loeffler's endocarditis
- scarlet fever
- irradiation
- during convalescence from any infection
- hypereosinophilic syndrome
- post-splenectomy
- cholesterol emboli syndrome
- drugs that may cause raised eosinophil count include (1,2,3,4):
- antimicrobials
- such as penicillins, cephalosporins, nitrofurantoin, tetracyclines, daptomycin, fluoroquinolones
- sulphonamides
- such as sulfasalazine, septrin, dapsone
- ranitidine
- allopurinol
- angiotensin converting enzyme (ACE) inhibitors
- anticonvulsants
- such as phenytoin, carbamazepine, lamotrigine
- anti-retrovirals
- nevirapine, abacavir
- non-steroidal anti-inflammatory drugs (NSAIDs)
- methotrexate
- interleukin-2 (IL-2)
- antimicrobials
If raised eosinophil count in an adult (3):
Factors such as intercurrent steroid treatment and bacterial or viral infection can transiently lower eosinophil counts (4)
Note *; Eosinophilic asthma, a subtype of asthma, involves the accumulation of eosinophils in the airways. These eosinophils release mediators and cytokines, contributing to severe airway inflammation and tissue damage. Emerging evidence now suggests that targeting eosinophils could reduce airway remodelling and slow the progression of asthma.
Although a standard definition of eosinophilic asthma remains elusive, clinical trials have utilized peripheral blood eosinophil counts of ≥150 cells/µL, ≥300 cells/µL, or ≥400 cells/µ, as well as sputum eosinophil levels exceeding 2 to 3%, to describe eosinophilic asthma and can readily be identified in a primary care setting.(5,6)
Reference:
- Ramirez GA et al. Eosinophils from Physiology to Disease: A Comprehensive Review. Biomed Res Int. 2018;2018:9095275
- Kovalszki A, Weller PF. Eosinophilia. Prim Care. 2016 Dec;43(4):607-617.
- NHS Camden CCG. Abnormal FBC guidance - for adults
- Thakker C, Booth H L, Lambert J, Morgan S, Checkley A M. Investigating eosinophilia BMJ 2023; 380
- Skolnik, N.S.; Carnahan, S.P. Primary care of asthma: New options for severe eosinophilic asthma. Curr. Med. Res. Opin. 2019, 35, 1309–1318.
- Levy, M.L et al. Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update. npj Prim. Care Respir. Med. 2023, 33, 7
Related pages
- Atopy
- Angioneurotic oedema
- Helminthic diseases
- Polyarteritis nodosa
- Churg-Strauss syndrome
- Pemphigus
- Dermatitis herpetiformis
- Hodgkin's disease
- Addison's disease
- Leukaemia (eosinophilic)
- Chronic myeloid leukaemia
- Loeffler's syndrome
- Eosinophilic endomyocardial disease
- Hypereosinophilia syndrome
- Roundworms
- Scarlet fever
- Splenectomy
- Cholesterol emboli syndrome
- Drug-induced eosinophilia
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.